| Medically reviewed by
Robin Backlund, BHSc
Last update:

Blood pressure is the force exerted by blood flow against artery walls, measured as systolic (during heartbeats) and diastolic (between heartbeats) pressure.
Lowering high blood pressure is crucial because it is closely linked to a heightened susceptibility to cardiovascular conditions such as myocardial infarctions, cerebrovascular accidents, and cardiac insufficiency.
As per American Heart Association (AHA) guidelines, blood pressure is categorized as high when it exceeds 120/80, ranging from elevated levels to a hypertensive crisis if it goes above 180/120.
Prolonged elevation of blood pressure can exert stress on the heart and harm the integrity of blood vessels, resulting in atherosclerosis (a condition where the narrowing and stiffening of arteries occur).
Certain individuals are at a higher risk of developing high blood pressure. These include individuals with a family history of hypertension, those who are overweight or obese, people who consume excessive amounts of sodium (salt) in their diets, and individuals who lead sedentary lifestyles.
The main factor in lowering blood pressure is the reduction of systemic vascular resistance (SVR) within the circulatory system.
According to the 2008 book Essentials of Cardiac Anesthesia, published by Dr. Joel A Kaplan, SVR refers to the resistance encountered by blood flow as it passes through the arteries and arterioles throughout the body.
When SVR decreases, it results in less force exerted by blood against the arterial walls, ultimately leading to a decrease in blood pressure.
Various mechanisms, including the relaxation of vascular smooth muscle, vasodilation, and changes in blood vessel diameter, contribute to the reduction in SVR.
While SVR is a critical clinical gauge, diet plays a pivotal role in blood pressure management. The main dietary consideration is reducing sodium intake, as excessive salt consumption can lead to water retention and increased blood pressure.
Apart from diet, lifestyle modifications play a significant role in lowering blood pressure. Regular physical activity, such as aerobic exercise, can improve heart health and reduce hypertension risk. Lifestyle habits like smoking cessation and moderate alcohol consumption are essential for maintaining healthy blood pressure levels.
One of the main dangers associated with high blood pressure is its potential to damage vital organs, including the heart, brain, kidneys, and blood vessels.
Over time, this damage can lead to heart attacks, strokes, kidney disease, and other life-threatening conditions.
Common symptoms of high blood pressure are often absent or subtle, earning it the silent killer moniker. However, some individuals may experience headaches, dizziness, blurred vision, or nosebleeds.
The primary cause of high blood pressure is multifactorial and may involve genetic predisposition, lifestyle choices, and underlying medical conditions.
Regular monitoring is an effective way to keep high blood pressure under check, and using the best blood pressure monitor available in the market will help you obtain clinically valid information about your heart’s status.
Factors such as obesity, a sedentary lifestyle, high salt intake, excessive alcohol consumption, and stress all contribute to the development of hypertension.
Genetics can also influence your susceptibility to high blood pressure, making it important to consider family history when assessing risk.
While some factors are not within our control, there are 16 methods that you can follow and include in your daily life to lower hypertension, as explained below.
Contents
1. Reduce your salt intake
Sodium, a component of table salt, is an essential mineral for bodily functions, but excessive consumption can lead to increased blood pressure.
This occurs because sodium holds onto water, increasing the volume of blood inside the blood vessels, which raises blood pressure.
The popular ELSA-Brasil study, published in Nature in 2022, which studied over 9,028 participants, found significant direct and BMI-mediated effects of salt intake on both SBP and DBP in individuals without hypertension.
Extensive research, including studies like the landmark DASH (Dietary Approaches to Stop Hypertension) and the findings of the Centers for Disease Control and Prevention (CDC), have consistently shown a strong link between high sodium intake and elevated blood pressure levels.
The AHA advises that healthy adults should aim to restrict their daily sodium intake to a maximum of 2,300 milligrams, with an ultimate target of ideally not exceeding 1,500 mg per day for most individuals.

To lower your sodium intake, it’s advisable to scrutinize nutritional labels, decrease your consumption of processed and restaurant-prepared meals, choose herbs and spices as alternatives for seasoning instead of salt, and select fresh fruits and vegetables over canned ones.
Foods like processed meats, canned soups, pizza, cheese, and salty snacks are high in sodium include.
Rather, choose healthier foods like fresh meats, homemade soups with low-sodium broth, homemade pizza with fresh toppings, unprocessed cheeses, and snacks like unsalted nuts or fresh fruits and vegetables.
By making these changes, individuals can effectively lower their sodium intake, which can significantly help in managing and reducing blood pressure.
2. Eat healthy foods
Consuming nutritious meals is a comprehensive approach that involves integrating a variety of healthy foods into one’s diet to manage and lower blood pressure.
This method affects blood pressure by supplying the body with essential nutrients, such as potassium and magnesium, which are known to help relax blood vessels and reduce blood pressure.
While there’s no specific quantity for too much when it comes to nutritious food, balance, and moderation are key. Overeating, even healthy foods, can lead to weight gain, which is a risk factor for high blood pressure.
Shocking findings were revealed in a 2021 study published in the Annals of Translational Medicine by Yan Chen et al., which reported that the incidence of high blood pressure among college students is on the rise, with 12% currently experiencing high blood pressure due to poor eating habits.
The AHA and WHO also advocate for nutritious eating patterns for cardiovascular health, putting more stress on a diet rich in fruits, vegetables, and low-fat dairy.
To incorporate more nutritious meals, you can start by increasing the intake of whole grains, lean proteins, and a variety of fruits and vegetables while reducing the consumption of processed foods, which are often high in sodium and unhealthy fats.
You can avoid less healthy options by swapping out white bread for whole-grain varieties, choosing baked or grilled proteins instead of fried, and opting for fresh fruits over sugary desserts.
3. Avoid refined carbs and sugar
Refined carbohydrates and added sugars are prevalent in many modern diets, often found in foods like bread, pasta, snacks, and sweetened beverages.
Excessive consumption of these constituents can exert a notable impact on blood pressure by inducing a swift elevation in both blood sugar and insulin levels. This, in turn, contributes to heightened blood pressure.
The AHA recommends limiting added sugars to no more than 6 teaspoons (24 grams) per day for women and 9 teaspoons (36 grams) for men.

A study published by Dr. James J DiNicolantonio and his colleague in the Open Heart Journal reports that, beyond salt, added sugar can cause damage to the heart, leading to hypertension and other cardiometabolic diseases.
In fact, leading health moderators like the WHO and the CDC have also acknowledged this relationship.
To mitigate these effects, individuals can adopt simple strategies such as reading food labels to avoid hidden sugars, opting for whole grains over refined carbs, and incorporating more fresh fruits and vegetables into their diets.
Foods particularly high in processed carbohydrates and added sugars include candy, cookies, sugary cereals, and white bread.
Healthier alternatives are available, such as whole fruits instead of sugary snacks and whole-grain or legume-based pasta instead of traditional white pasta.
4. Consider trying the DASH diet
The DASH diet, an acronym for Dietary Approaches to Stop Hypertension, is a nutrition strategy created to help manage high blood pressure.
It focuses on a diet rich in fruits, vegetables, whole grains, and lean protein sources while limiting salt, red meat, sugary treats, and fatty foods.
The diet aims to lower blood pressure by enhancing the consumption of essential nutrients such as potassium, calcium, and magnesium, which help in expanding blood vessels and softening the arteries.
Its benefits extend beyond blood pressure reduction, also aiding in weight loss and improved cardiovascular health.
In fact, there is a comprehensive guide published by the National Heart, Lung, and Blood Institute (NHLBI), which, in the public interest, streamlines and provides a guide to lower blood pressure through diet management, lifestyle modification, and physical activities.
Adherence to the DASH diet typically involves consuming 4-5 servings of both fruits and vegetables, 6-8 servings of whole grains, and 2-3 servings of low-fat dairy products daily.
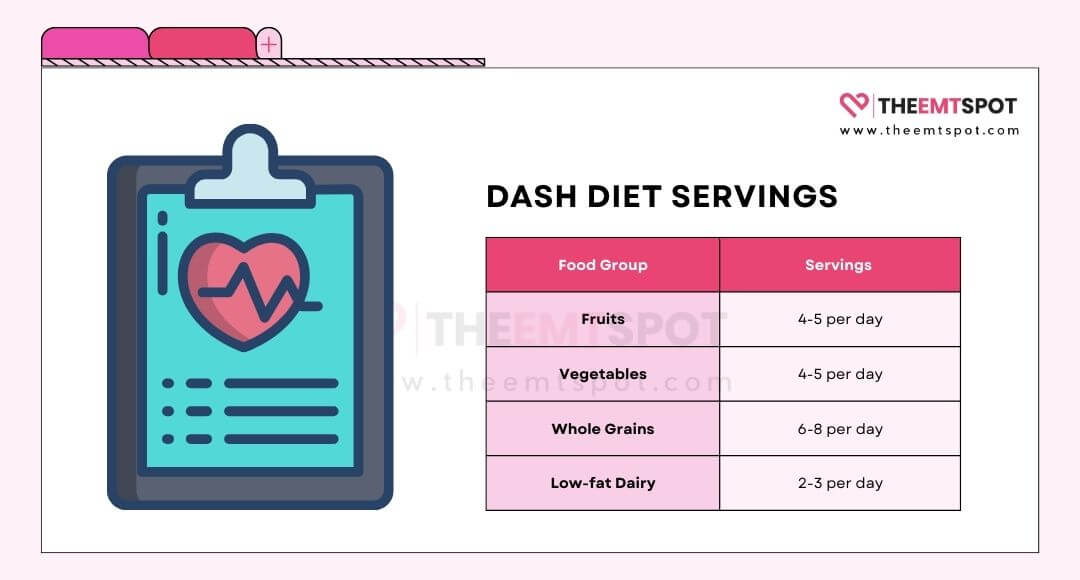
Lean meats, fish, and nuts are also integral but in moderation. While the DASH diet is predominantly beneficial, possible side effects can include initial feelings of fatigue or dizziness due to the sudden decrease in sodium.
There’s also potential for medication interaction, particularly with diuretics and blood pressure medications, which could lead to excessively low blood pressure.
To start the DASH diet, it’s advisable to gradually introduce dietary changes, initially focusing on reducing sodium intake and progressively incorporating the recommended food groups and servings.
Consulting with your doctor or a dietitian can provide personalized guidance and ensure a safe and effective transition.
5. Drink water
Maintaining proper hydration by drinking water is a simple yet effective method for managing blood pressure.
When the body is well-hydrated, the blood maintains a lower viscosity, which facilitates smoother blood flow through the arteries, thereby reducing the pressure exerted on arterial walls.
The benefits of staying hydrated include better blood pressure control and enhanced kidney function, which plays a critical role in blood pressure regulation by managing fluid balance and electrolyte levels in the body.
Hydration is important, but a study published in 2019 by Naser et al. in the Journal of the American Heart Association suggests that consuming water rich in minerals such as potassium (K+), calcium (Ca2+), and magnesium (Mg2+) may lower blood pressure.
To aid in hydration, foods with high water content, such as cucumbers, tomatoes, and watermelons, are recommended, with a suggested serving of at least eight 8-ounce glasses of water per day, commonly known as the 8×8 rule.

Although there are few adverse effects associated with maintaining proper hydration, consuming excessive amounts of water can result in water intoxication or hyponatremia, a serious condition characterized by abnormally low sodium concentrations in the blood.
There are also potential medication interactions, particularly with diuretics, which increase urine production. Individuals on such medications should consult a doctor or a dietitian to tailor their water intake accordingly.
6. Eat dark chocolate
Dark chocolate, characterized by its high cocoa content and minimal processing, has been linked to various health benefits, particularly in the realm of cardiovascular well-being.
It contains flavonoids, which are natural compounds that can help dilate blood vessels, thereby reducing blood pressure.
These flavonoids stimulate the endothelium( the lining of arteries) by producing Nitric Oxide (NO), which sends signals to the tiny muscles around the arteries, instructing them to relax. This relaxation eases the resistance to blood flow and thus reduces blood pressure.
The benefits of dark chocolate are not just anecdotal; numerous studies have underscored its efficacy.
An Australian study conducted by the National Institute of Integrative Medicine, led by Prof. Karin Ried and her colleagues, suggests that there is a significant reduction in blood pressure in people who use cocoa or dark chocolate, with an average decrease of 4.0/1.98 mmHg.
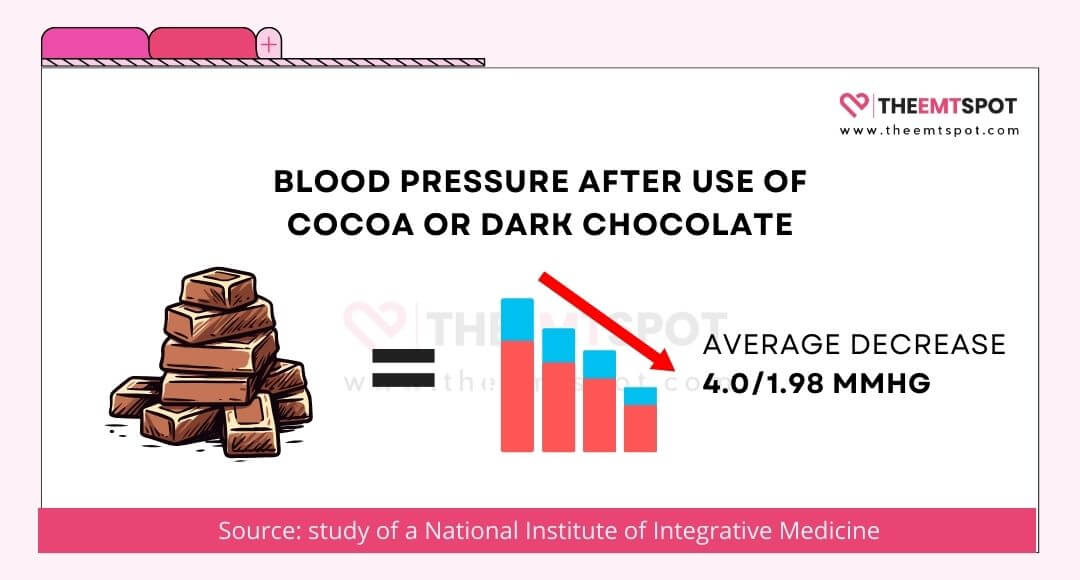
The AHA, after reviewing various studies, highlighted that the polyphenols in cocoa could decrease both systolic and diastolic blood pressure by a significant margin.
The suggested serving of dark chocolate is around one to two ounces per day. Exceeding this could lead to negative effects due to the high-calorie content, potentially leading to weight gain and diminishing the positive impacts on blood pressure.
Additionally, overindulgence can lead to caffeine-related side effects such as restlessness and a rapid heartbeat. Thus, dark chocolate can be a delightful addition to a heart-healthy lifestyle.
7. Experiment with these herbs
Herbal remedies have been a cornerstone of natural medicine for centuries, and a regional treatment regime exists in every country based on their local herbs.
A study published in Pharmacognosy Reviews in 2011 found that 75-80% of the world’s population still uses herbal supplements for various ailments, with cardiac care being a major niche.
The authors have also included a comprehensive list of all major herbal medicines and their effects on hypertension in this review publication.
- Buchu, native to South Africa, contains compounds believed to have diuretic properties, potentially aiding in excreting excess water and salt, which can consequently reduce blood pressure. However, its efficacy for hypertension hasn’t been verified in human studies.
- Garlic, another herb, has shown promise in studies, with findings suggesting that 300 mg of dried garlic extract can help reduce systolic and diastolic blood pressure in hypertensive individuals.
- Prickly custard apple, also known as soursop, has also been historically used for hypertension, with recent studies showing potential blood pressure reduction when supplemented.
- Celery’s potential in blood pressure regulation is attributed to a natural chemical called 3-n-butylphthalide. Although animal studies have shown promise, human trials remain inconclusive.
- Basil, integral to traditional Chinese medicine for cardiovascular issues, contains eugenol, a compound linked to lowered blood pressure. Preliminary studies on basil supplements have shown potential antihypertensive benefits, but concrete evidence is still lacking. Exact servings may vary depending on the herb and individual needs. Overconsumption can pose risks, so it’s essential to consult your doctor before incorporating these herbs into one’s diet.

While these herbs offer potential benefits, they may also come with side effects such as diarrhea, palpitations, insomnia, kidney malfunction, etc., underscoring the importance of moderation and supervision.
8. Follow prescribed medications
Taking prescription medication involves the use of drugs that are provided under the authority of a medical professional to treat, cure, or prevent various health conditions.
When it comes to blood pressure, certain prescription medications are specifically designed to regulate or lower it.
These medications can be highly beneficial, particularly for individuals suffering from hypertension, as they help in preventing heart disease and strokes.
Popular blood pressure medications include ACE inhibitors like Lisinopril, Angiotensin II receptor blockers (ARBs) such as Losartan, Beta-blockers including Atenolol, Calcium channel blockers like Amlodipine, Diuretics such as Hydrochlorothiazide, and Renin inhibitors like Aliskiren, each with unique mechanisms and considerations for managing hypertension.
The effectiveness of these drugs is well-established; they work through various mechanisms, such as dilating blood vessels or reducing the volume of blood, thereby lowering blood pressure.
The proof of their efficacy is backed by numerous research studies and clinical trials.
The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) is one of the largest studies which began in 1994 and lasted till 2002 with the support and financial backing from the NHLBI.
The trial concluded that diuretics are as effective as calcium channel blockers, ACE inhibitors, and alpha-adrenergic blockers in managing high blood pressure and preventing cardiovascular events, recommending diuretics as the first-line treatment.
Suggested servings or dosages of these medications are highly individualized, depending on the specific drug, the severity of hypertension, and the patient’s overall health profile.
It’s crucial to adhere to the prescribed amount since taking more than recommended can lead to adverse effects such as hypotension, kidney damage, or electrolyte imbalances.
Possible side effects vary based on the medication but can include dizziness, headaches, and gastrointestinal issues.
Therefore, it’s imperative to take these medications exactly as prescribed and under the supervision of a doctor.
Medication | What It Does | Side Effects |
Diuretics | Flushes out extra water and sodium. | · Dehydration · Erectile dysfunction · Weakness, cramping and fatigue · Onset of gout or intense foot pain |
Beta Blockers | Makes your heart beat with less intensity. | · Asthma and breathing issues · Depression · Sleep disturbances · Erection problems · Cold feet and hands |
ACE Inhibitors | Relaxes blood vessels by blocking the formation of the hormone that narrows the blood vessels. | · Dry, hack cough · Skin rash · Loss of taste |
ARBs | Protect blood vessels from narrowing and keeps them open. | · Dizziness |
CCBs | Prevent calcium from entering the heart, muscle and blood cells. | · Constipation · Headaches · Dizziness · Swollen ankles · Palpitations |
Alpha-Blockers | Lessen the nerve impulse to narrow blood vessels. | · Dizziness · Light-headedness · Quick pulse |
Alpha-2 Receptor Agonist | Reduces adrenaline production in the nervous system. | · Drowsiness · Dizziness |
Alpha-Beta-Blockers | Reduce nerve impulses to slow down heartbeat. | · Low blood pressure · Dizziness · Light-headedness · Weakness |
Central Agonists | Control nerve impulses to relax blood vessels. | · Anemia · Constipation · Dizziness · Dry mouth · Drowsiness and weakness · Erection problems · Fever |
Peripheral Adrenergic Inhibitors | Blocks neurotransmitters in the brain to relax smooth muscles. | · Diarrhea · Heartburn · Congested nose · Dizziness and weakness |
Vasodilators | Relax muscle walls to allow blood to flow better through blood vessels. | · Excessive hair growth · Headaches · Water retention · Joint aches and pains · Palpitations · Eye swelling |
Renin Inhibitor | Decreases the chemicals that tighten blood vessels. | · Cough · Diarrhea · Stomach pain · Heartburn · Rash |
9. Consider using vitamins and supplements
Vitamins and other supplements are concentrated sources of nutrients with a nutritional or physiological effect.
They’re intended to supplement the diet and are not considered drugs. Regarding blood pressure, certain vitamins like Vitamin D and mineral supplements like magnesium have been associated with blood pressure regulation.
For instance, magnesium helps relax blood vessels, potentially lowering blood pressure.
The benefits of vitamins and supplements extend beyond blood pressure regulation; they can also bolster the immune system, improve bone health, and compensate for dietary deficiencies.
However, the effectiveness of vitamins and supplements can vary widely. Factors such as bioavailability, individual health conditions, and the presence of other nutrients can influence their efficacy.
Substantial research backs the benefits of some supplements; for example, Vitamin D’s role in bone health is well-supported by studies and institutions like the National Institutes of Health (NIH).
However, not all supplements have a strong evidence base, and some claims may be based on limited or anecdotal evidence.
Suggested servings for vitamins and supplements are typically provided by health authorities like the Food and Drug Administration (FDA) or the NIH and are often found on product labels.
Exceeding these recommendations can lead to toxicity. For instance, too much Vitamin A can cause liver damage, while excessive Vitamin D can lead to calcium buildup in the blood.
Possible side effects of vitamins and supplements can range from mild, like nausea or headache, to severe, including organ damage or interactions with medications.
10. Manage your body weight
Maintaining a healthy body weight is defined as having a body mass index (BMI) that falls within the range considered normal, typically between 18.5 and 24.9.
This balance between height and weight is crucial for overall health, especially for blood pressure regulation.
Higher body weight can lead to increased strain on the heart, causing higher blood pressure, while a healthy weight often correlates with normalized blood pressure levels.

There are many perks to maintaining a healthy body weight, ranging from reduced risk of chronic diseases like diabetes and heart disease to improved mental health and mobility.
The Framingham Heart Study, funded by NHLBI, is a long-term, ongoing cardiovascular cohort study that began in 1948 to study patterns of cardiovascular and other diseases.
Research involving 14,000 residents of Framingham, Massachusetts, has indicated that overweight individuals face a substantially greater risk of heart disease development when compared to those who maintain a healthy weight.
To embark on the journey towards a healthy body weight, it is recommended to start with small, sustainable changes.
These include incorporating more whole foods like fruits, vegetables, and lean proteins into the diet, increasing physical activity gradually, and seeking support from healthcare professionals or weight management programs when necessary.
Mindful eating practices and keeping a food diary can also be beneficial in making more informed choices about nutrition and portion sizes.
However, what many are unaware of is that stress can contribute to weight gain and have both direct and indirect effects on hypertension.
11. Reduce stress
Stress is a notable contributor to high blood pressure; when you’re stressed, your body is in a constant state of ‘fight or flight’, producing stress hormones which increase your heart rate and constrict your blood vessels, thus raising your blood pressure.
Below are some of the facts that will help you understand stress better and, thereby, regulate it effectively.
- Direct impact on heart health: Techniques like deep breathing, meditation, and mindfulness activate the parasympathetic nervous system. Activation of this system helps slow the heart rate and lower blood pressure.
- Supported by research: The effectiveness of stress reduction in managing hypertension is supported by research and health institutions. Harvard Health Publishing states that reducing stress can directly impact blood pressure levels, aiding hypertensive patients.
- Worldwide recognized practice: The American Heart Association (AHA), World Health Organization (WHO), Centers for Disease Control and Prevention (CDC), and National Heart, Lung, and Blood Institute (NHLBI) all strongly recommend managing stress alongside medications for reducing high blood pressure.
- Dual benefits: Reducing stress levels significantly impacts weight loss, thereby promoting your general health, and also helps reduce the prevalence, incidence, and severity of hypertension.
- Easily achievable: Unlike other health concerns, stress can easily be controlled through practices such as meditation, breathing techniques, yoga, mindfulness, improving sleep, cognitive behavioural therapy, etc., without even requiring medication.
- Simple to start: You don’t need elaborate preparation to include this in your daily life. The steps below will give you an idea of how to incorporate it.
- Start with small, manageable practices like dedicating a few minutes daily to deep breathing or mindfulness exercises.
- Gradually building these habits can contribute to long-term blood pressure control and overall well-being.
- Breathing techniques, on their own, can be easily integrated into your current lifestyle to help manage stress.

12. Exercise regularly
Regular physical activity is a structured exercise regimen or any bodily movement that enhances or maintains physical fitness and overall health.
Engaging in regular physical activity can significantly affect blood pressure levels, often contributing to a decrease in both systolic and diastolic measurements.
The benefits of such activity are manifold, including strengthening the heart muscle, improving blood circulation, and reducing stress levels, all of which collectively contribute to lower blood pressure.
The AHA suggests a weekly exercise regimen that consists of either 2.5 hours of moderate-intensity aerobic activity, 1.2 hours of vigorous-intensity activity, or a combination of these, along with muscle-strengthening exercises on two or more days per week.
According to a 2022 Nature study, “A single session of exercise reduces blood pressure reactivity to stress: a systematic review and meta-analysis,” even a single session of strenuous workout reduces blood pressure in younger adults.
A variety of physical activities are recommended for blood pressure management. These include aerobic exercises like brisk walking, swimming, cycling, or jogging, which help improve heart and lung fitness.
Strength training workouts, such as weight lifting, can also assist in maintaining healthy blood pressure.
To begin with, combine physical activity into your routine and begin with gradual increments. If new to exercise, start with short, 10-minute sessions and progressively build up the duration and intensity.
Choosing activities you enjoy is essential, which will help ensure consistency and long-term adherence.
Please do not forget to consult your doctor or a trained physician, as there has been an increase in incidents of death associated with physical exertion at gyms, often due to inadequate health assessments.
13. Get good sleep
Lowering blood pressure is a vital health goal for many, and ensuring a restful night’s sleep can be a significant contributor to this aim.
Sleep enables the body to control stress hormones and assists in maintaining a healthy nervous system, both of which are essential for regulating blood pressure levels.
A restful night’s sleep offers advantages such as enhanced mood, improved cognitive function, and a reinforced immune system, all of which indirectly contribute to cardiovascular well-being.
CDC recommends that adults should get at least 7 hours of uninterrupted sleep; otherwise, it may increase the risk of hypertension.
A study by David A. Calhoun, MD, and Susan M. Harding, MD, FCCP, published in the journal Chest, suggests that cardiovascular disease is elevated if blood pressure does not decrease during sleep.
Sleep quality plays a critical role in determining this dip in blood pressure.

Recommended practices include establishing a regular sleep schedule, creating a restful environment free from noise and light pollution, and avoiding stimulants like caffeine close to bedtime.
Other strategies to initiate this habit include participating in relaxing activities before bedtime and designating your bedroom exclusively for sleep, reinforcing the mental connection between space and rest.
You can take a significant step towards managing their blood pressure and improving their overall health by prioritizing sleep hygiene.
14. Limit alcohol intake
Restricting alcohol intake is a recognized approach to managing hypertension, a condition characterized by persistently high blood pressure.
Alcohol can cause a significant and immediate rise in blood pressure, even in moderate amounts.
Reducing alcohol consumption can have a beneficial effect on blood pressure, often leading to a noticeable decrease in hypertensive individuals.
A popular study published in The Lancet by Dr. Michael Roerecke, PhD, et al., found that a 50% reduction in alcohol intake in people who consume 6 or more drinks per day can decrease their systolic blood pressure by 5-6 mmHg and diastolic blood pressure by 4-4.5 mmHg.
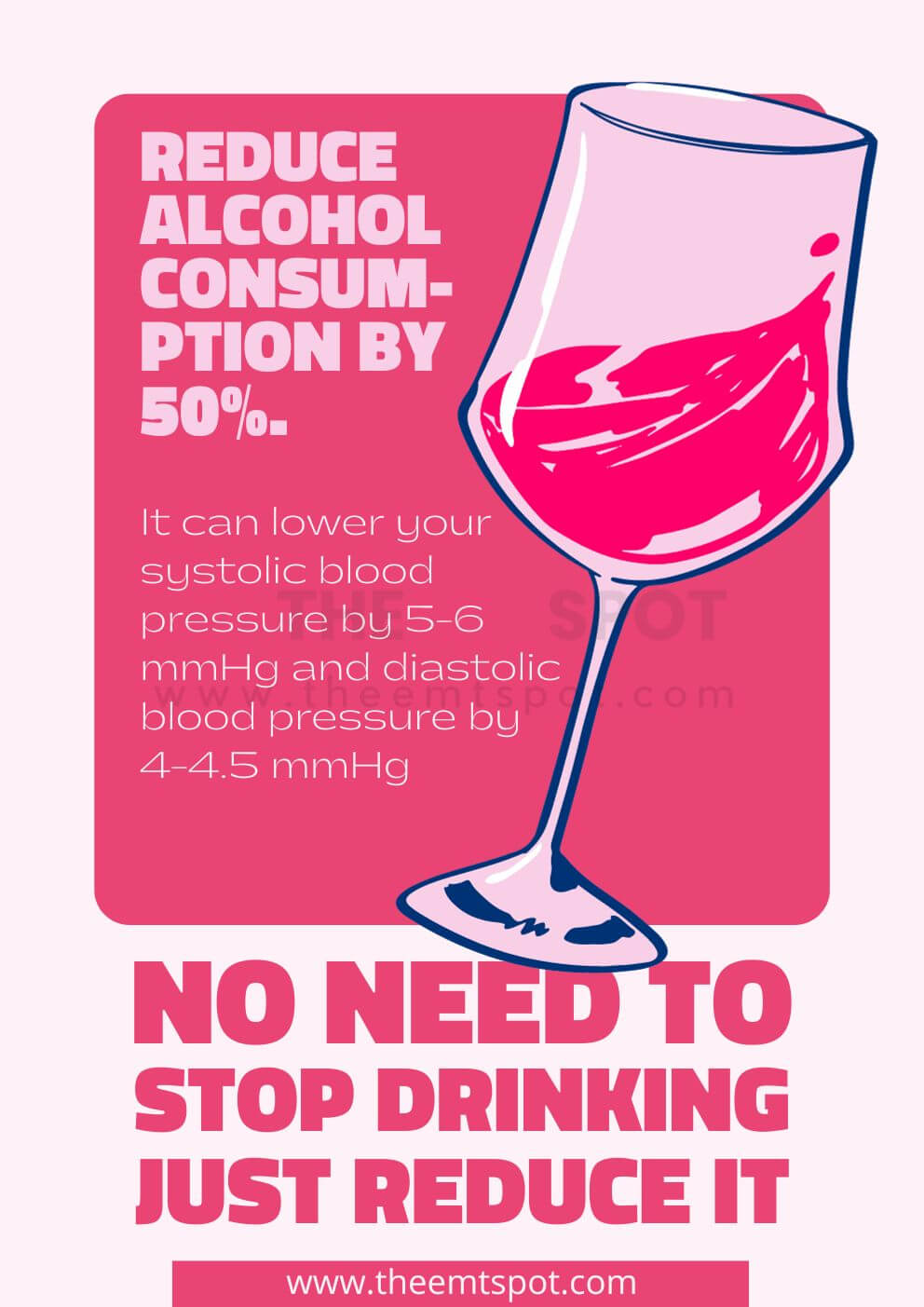
Moderation is key, with suggested servings typically capped at one drink a day for women and two for men, as defined by the U.S. Dietary Guidelines for Americans.
However, excessive intake can counteract these benefits, leading to a rebound effect that may exacerbate hypertension.
The threshold for too much varies individually but generally aligns with surpassing daily recommended limits.
Overconsumption of alcohol not only negates its antihypertensive effects but also poses other health risks, such as liver disease, addiction, and an increased likelihood of accidents.
Therefore, while restricting alcohol intake can be an effective tool in managing blood pressure, it is crucial to adhere to moderation to avoid adverse effects.
15. Quit smoking
Lowering blood pressure is a critical health goal for many, and kicking the smoking habit plays a pivotal role in achieving it.
Smoking cigarettes has a direct and adverse effect on blood pressure, causing an immediate spike due to the nicotine’s stimulatory effect on the cardiovascular system.
In the long term, it contributes to the hardening of arteries and a sustained increase in blood pressure.
Abstaining from smoking offers a multitude of benefits, including reduced blood pressure, decreased heart disease risk, and improved overall cardiovascular health.

According to the AHA, smoking is directly linked to an elevated risk of hypertension. Additionally, even passive smoking is associated with increased plaque buildup in the arteries, leading to a condition known as atherosclerosis.
However, strangely, a study published in the AHA journal Hypertension titled “Effects of Smoking Cessation on Changes in Blood Pressure and Incidence of Hypertension” suggests that the longer the cessation, the greater the increase in blood pressure.
While there are a few studies that may seem counterintuitive, the majority of studies suggest a positive correlation between smoking cessation and a reduction in hypertension.
Unlike dietary changes or medications, there are no suggested “servings” or doses when it comes to smoking cessation; the goal is complete abstinence.
While there is no risk of “too much” quitting, the process can have side effects, including nicotine withdrawal symptoms like irritability, cravings, and weight gain.
However, these side effects are temporary and generally considered minor when compared to the long-term health benefits of quitting smoking.
16. Cut back on caffeine
Caffeine, a common stimulant present in items such as coffee, tea, chocolate, etc., has the potential to trigger a brief yet significant elevation in your blood pressure levels, regardless of whether you are typically prone to hypertension or not.
The precise way caffeine does this isn’t fully understood, but it’s believed to block a hormone that helps keep your arteries widened, or it might cause your adrenal glands to release more adrenaline, which causes blood pressure to increase.
Despite its temporary effects, there’s scant evidence to suggest that caffeine has long-term effects on blood pressure, especially for habitual drinkers, as a tolerance to its effects may develop.
According to the European Society of Hypertension and the European Society of Cardiology, the quality of most studies is insufficient to issue a firm recommendation or discouragement of coffee consumption.
The European Food Safety Authority (EFSA) observed that caffeine consumption can induce a temporary mean increase in systolic and diastolic BP, but there is high inter-individual variability, and the BP generally returns to baseline after about 2 to 4 hours.
Despite this, doctors recommend keeping caffeine intake within safe limits, especially for those with hypertension.
The FDA states that 400 milligrams per day of caffeine is generally safe for most people, which includes those with high blood pressure.
Recommended sources of low-caffeine beverages include herbal teas and decaffeinated coffee. When starting to reduce caffeine intake, it’s beneficial to gradually decrease consumption to avoid withdrawal symptoms like headaches and irritability.
For instance, you can mix regular coffee with decaffeinated coffee and slowly increase the proportion of decaf over time or opt for smaller servings of caffeinated beverages.
How to lower blood pressure while pregnant?
Lowering blood pressure during pregnancy is vital for the well-being of both the mother and the baby. Ensuring regular prenatal care allows for careful monitoring of blood pressure and provides an opportunity for tailored guidance from healthcare professionals.
According to Prof. Jacquelyn McMillian-Bohler, Assistant Clinical Professor at Duke University School of Nursing:
“Hypertensive disorders typically affect about 5% to 10% of pregnancies overall, and they are the leading cause of maternal mortality.”
She added:
“So, epidemiologically speaking, it affects up to about 8% of pregnancies worldwide.”
Prof. Bohler continued:
“Now, among other patients who experience chronic hypertension, 41% will end up delivering via cesarean, 28% will experience a preterm birth, 25% to 40% will go on to develop preeclampsia, which is different. 21% will have a baby that ends up in the neonatal intensive care unit, 17% will experience a baby of low birth weight, and 4% will have a fetal death.”
Adopting a healthy diet rich in fruits, vegetables, whole grains, and lean proteins while limiting salt intake can be beneficial in managing blood pressure levels.
Engaging in doctor-approved physical activities and employing stress-reduction techniques such as prenatal yoga, meditation, or deep breathing can also contribute to maintaining healthy blood pressure.
Pregnant women should avoid tobacco, alcohol, and excessive caffeine, as these substances can elevate blood pressure and harm the pregnancy.
Monitoring weight gain to stay within recommended guidelines is another crucial aspect of managing blood pressure.
In some instances, medication may be prescribed to manage blood pressure effectively, but it is imperative to only take medicines under the guidance of a healthcare provider.
High blood pressure while pregnant can sometimes indicate more serious conditions like preeclampsia, necessitating prompt medical attention and intervention.
Follow the recommendations given by your obstetrician. It is essential to manage blood pressure during pregnancy for the health and safety of both the mother and child.
How can I lower blood pressure in my children?
To lower blood pressure in children, a multifaceted approach often centered around lifestyle modifications is recommended, but it’s crucial to first consult a healthcare professional for personalized guidance.
- Initiating a balanced diet that emphasizes fruits, vegetables, whole grains, and lean proteins while limiting sodium, sugars, and saturated fats can be beneficial. A team of researchers from the University of Arkansas for Medical Sciences and Arkansas Children’s Hospital found that prehypertension is common in adolescents and poses a risk for future hypertension and cardiovascular disease.
- Encouraging regular physical activity is also essential, with experts suggesting at least 60 minutes of moderate to vigorous exercise daily for children aged 6–17 years.
- Monitoring and maintaining a healthy weight is important, as overweight and obesity are risk factors for hypertension.
- Reducing screen time can promote a more active lifestyle and help in weight management. Addressing stress through engaging in activities and ensuring adequate sleep are vital components, as both stress and insufficient sleep can negatively impact blood pressure.
- Lastly, routine health checkups are crucial for monitoring blood pressure and overall well-being.
In cases where a child is diagnosed with hypertension, consider consulting a pediatric cardiologist, as proper intervention is crucial in alleviating any impending dangers.
How long does it take for blood pressure to decrease?
The duration it takes for blood pressure to decrease can vary significantly based on the approach taken and individual health factors.
Lifestyle modifications like dietary adjustments, regular exercise, and stress management can lead to noticeable improvements in blood pressure within a few weeks to months, provided these changes are consistently adhered to over time.
On the other hand, medications prescribed for hypertension may start affecting blood pressure within hours to days, though it might take several weeks to witness their full impact.
According to Pritikin’s Medical Director, Danine Fruge, MD (source: www.pirtikin.com)::
“We have many people with hypertension who come to Pritikin, and within three days, many have blood pressures that have dropped so low that we need to reduce their medications or take them off their pills altogether.”
He added:
“Yes, just three days. That’s how quickly and powerfully our bodies respond to healthy food, exercise, and other lifestyle changes.”
“I used to think these dramatic drops in blood pressure were something that happened to only a very few people,” continues Dr. Fruge, “but I’ve been here at Pritikin for more than 15 years, and I see results like these every week. This isn’t a miracle. It’s simply what happens when we start taking good care of ourselves.”
In urgent situations, such as a hypertensive crisis, intravenous medications can rapidly lower blood pressure within minutes to hours.
It’s crucial to work closely with a healthcare professional to tailor a treatment plan, as responses can differ based on each person’s health status, the severity of their hypertension, and the chosen treatment method.
Continuous monitoring and potential adjustments to the treatment regimen are often necessary for effective blood pressure management. But what if you want to lower the blood pressure immediately?
How to lower blood pressure instantly?
Lowering blood pressure instantly can be challenging, as most methods for managing blood pressure are gradual.
However, in moments of acute stress or anxiety, some of the following approaches may help lower blood pressure slightly and temporarily.
According to an instruction set prepared by Nutritionist and Medical Writer Jenny Hills, the following approaches might be useful for instantly reducing blood pressure.
- Sit down and take deep breaths: Deep breathing can activate the parasympathetic nervous system and may help lower blood pressure.
- Practice relaxation techniques: Techniques like meditation, mindfulness, or progressive muscle relaxation can reduce stress and potentially lower blood pressure.
- Lay on your left side: This position can take some pressure off the vena cava, the body’s main vein, helping with circulation.
- Take a warm bath or shower: The warmth can help relax your muscles and dilate your blood vessels, potentially lowering blood pressure.
- Avoid stimulants: Stay away from caffeine and nicotine, which can temporarily raise blood pressure.
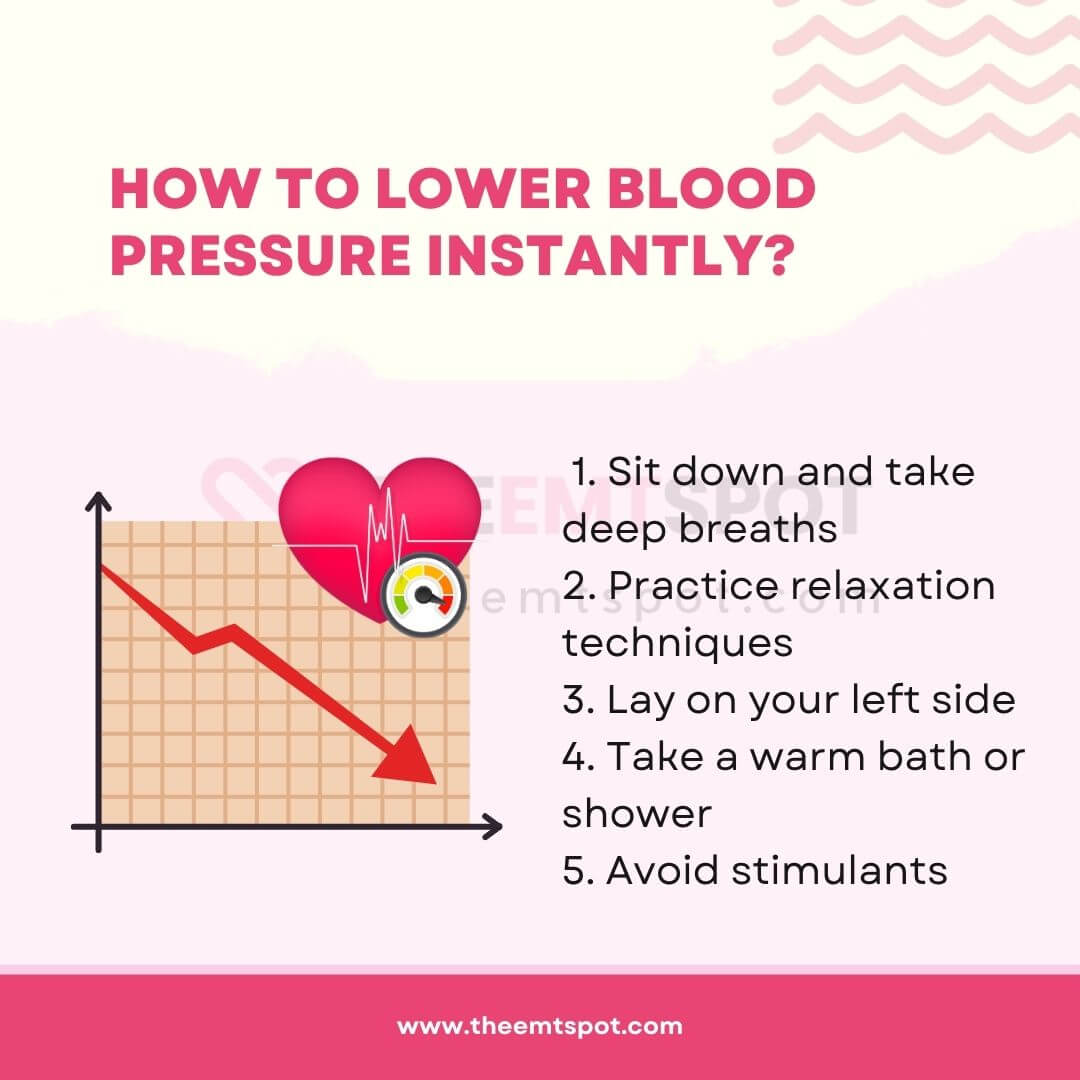
It’s important to note that these methods may not have a significant impact and are not substitutes for medical treatment.
Living with high blood pressure is risky due to the associated dangers and risks. Therefore, it is always recommended to monitor it regularly.
What are the dangers and risks of hypertension?
The dangers and risks of hypertension are well-documented, and it can be life-threatening in many cases. According to the Mayo Clinic review, below elaborated are some of the dangers associated with hypertension.
- Heart disease and heart attack: High blood pressure can lead to hardening and thickening of the arteries (atherosclerosis), which can result in a heart attack.
- Stroke: Hypertension can cause blood vessels in the brain to clog more easily or even burst, leading to a stroke.
- Heart failure: The increased workload from high blood pressure can cause the heart to enlarge and fail to supply blood to the body.
- Kidney disease or failure: Hypertension can damage the arteries around the kidneys and interfere with their ability to filter blood effectively.
- Vision loss: High blood pressure can strain or damage blood vessels in the eyes.
- Sexual dysfunction: This is more common in men with hypertension and can manifest as erectile dysfunction.
- Peripheral artery disease (PAD): Hypertension can narrow blood vessels in the legs, leading to pain, cramps, and fatigue while walking.
- Aneurysms: Increased blood pressure can cause blood vessels to weaken and bulge, forming aneurysms. If an aneurysm ruptures, it can be life-threatening.
- Cognitive changes: Uncontrolled high blood pressure may also affect your ability to think, remember, and learn. Trouble with memory or understanding concepts is more common in people with high blood pressure.
- Metabolic syndrome: This syndrome is a cluster of disorders of your body’s metabolism, including increased waist circumference, high triglycerides, low high-density lipoprotein (HDL) cholesterol, high blood pressure, and high insulin levels.
If you can identify the symptoms and perform a self-diagnosis, it will help you reach out to a doctor as soon as possible. The following section will help you understand the clinical symptoms of hypertension.
What are the symptoms of high blood pressure?
Symptoms of high blood pressure are often not present, especially in the early stages of hypertension.
Visible symptoms are typically exhibited during a hypertensive crisis stage, by which point it may already be too late.
According to AHA guidelines and practices, below are a few points that can help you identify hypertension at an early stage.
- Most of the time, high blood pressure has no symptoms.
- It’s important to note that not everyone with hypertension will necessarily experience symptoms such as nervousness, sweating, sleep difficulties, or facial flushing.
- In some individuals, high blood pressure may not result in headaches or nosebleeds. However, as the level of hypertension increases, these symptoms may become more apparent.
- Some symptoms may be indirectly related to high blood pressure but are not always caused by it, such as blood spots in the eyes, facial flushing, and dizziness.
- Frequent palpitations may sometimes be attributed to high blood pressure.
- Severe exhaustion and tiredness in your mid-40s might point to hypertension.
- In some cases, subconjunctival hemorrhage or a red spot on the eye can be observed.
Once you are familiar with the symptoms, it becomes easier to monitor your health. Understanding the causes will further increase your health consciousness and help you make wiser life choices.
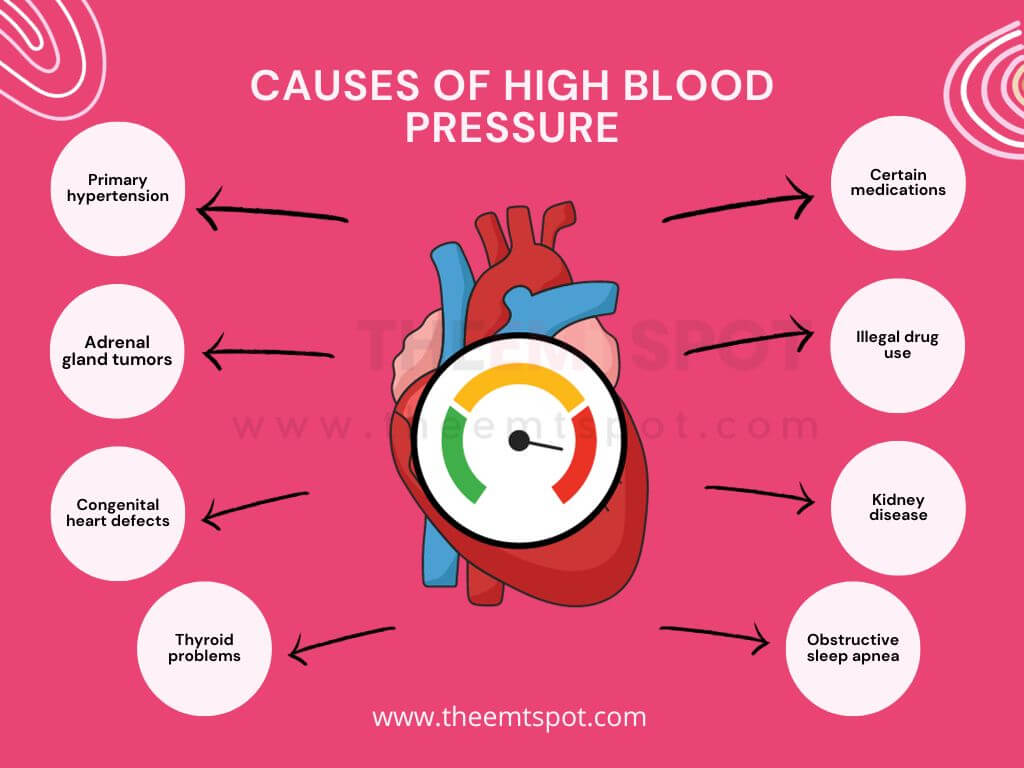
What are the causes of high blood pressure?
What causes high blood pressure? Various experts have attempted to answer this question in different ways, but the answers often remain the same.
According to Penn Medicine at the University of Pennsylvania Health System, the below factors are the causes of hypertension.
- Primary hypertension: Typically has no identifiable cause and develops gradually over many years.
- Adrenal gland tumors: Growths on the adrenal glands can disrupt hormone balance, raising blood pressure.
- Congenital heart defects: Structural problems in the heart present from birth can affect blood flow and pressure.
- Certain medications: Some drugs, including over-the-counter ones, can elevate blood pressure.
- Illegal drug use: Stimulants like cocaine and amphetamines can cause significant spikes in blood pressure.
- Kidney disease: The kidneys play a crucial role in regulating blood pressure, and disease can impair this function.
- Obstructive sleep apnea: Interrupted breathing during sleep can cause blood pressure to rise.
- Thyroid problems: Both hyperthyroidism and hypothyroidism can affect blood pressure.
Do you know that your dietary habits have a strong correlation with some of these causes? The next part of this article will provide you with insight into the relationship between food and hypertension.
What foods can cause high blood pressure?
All types of food can contribute to high blood pressure. As shocking as it may sound, this is indeed a fact.
Most unexpectedly, a study published in 2017 in the journal Advanced Nutrition revealed that commonly perceived healthy foods such as whole grains, refined grains, vegetables, fruits, nuts, legumes, eggs, dairy, and fish were found to increase blood pressure in a sample group.
However, this increase is dose-dependent, meaning it is related to the amount of food you consume.
One of the primary culprits is salt, or sodium, which is abundant in processed and packaged foods, canned soups, deli meats, and fast food.
Saturated and trans fats, found in fatty cuts of meat, full-fat dairy products, butter, and some baked goods, can also contribute to arterial plaque buildup, raising blood pressure.
Similarly, a high consumption of sugar and refined carbohydrates, prevalent in sodas, sweets, and white bread, can lead to weight gain, a known risk factor for hypertension.
Alcohol consumption, when excessive, can significantly increase blood pressure, and caffeine, present in coffee, tea, chocolate, and some soft drinks, may cause a temporary spike in some individuals.
Regular consumption of red meat, particularly processed varieties, is another factor due to its high saturated fat and sodium content.
Additionally, while fermented foods can offer health benefits, many pickled varieties are high in sodium, potentially increasing blood pressure.
Not just foods, even the choice of beverage has a strong influence on your blood pressure.
What drinks can cause high blood pressure?
Certain drinks can contribute to high blood pressure, and their usage and regulation are clearly mentioned in AHA, CDC, and NIH guidelines.
- Frequent or heavy drinking of alcoholic beverages may result in a prolonged elevation of blood pressure; thus, it’s essential to drink in moderation.
- Caffeinated drinks can cause short-term spikes in blood pressure, and their long-term effects remain somewhat ambiguous, though heavy, consistent intake may be a contributing factor.
- Sugary drinks, such as sodas and sweetened fruit punches, are linked to weight gain and obesity, which are prominent risk factors for hypertension.
- Energy drinks, often loaded with caffeine and other stimulants, can also elevate heart rate and blood pressure.
- Additionally, certain herbal teas and supplements, especially those containing licorice or ephedra, can have hypertensive effects.
It’s important to acknowledge that individual responses to these beverages can vary, and factors such as genetics, lifestyle, and overall dietary habits also play a crucial role in determining blood pressure.
What is a blood pressure chart, and how do you read it?
A blood pressure chart serves as a guide to evaluate whether your blood pressure readings indicate healthy levels or potential health issues.
As mentioned below, blood pressure is expressed in two numbers measured in millimeters of mercury (mmHg).
- Systolic pressure (the top number) indicates the arterial pressure as the heart beats.
- Diastolic pressure (the bottom number) represents the pressure during the heart’s rest between beats.
According to AHA guidelines, the normal reading is below 120/80 mmHg. Elevated blood pressure ranges from 120-129 mmHg systolic while maintaining a diastolic pressure below 80 mmHg.
High blood pressure is further categorized into stage 1, stage 2, and hypertensive crisis. If the two numbers fall into different categories, the higher one determines the blood pressure category.
For example, a 125/85 mmHg reading classifies as stage 1 hypertension because the diastolic number is in this range.
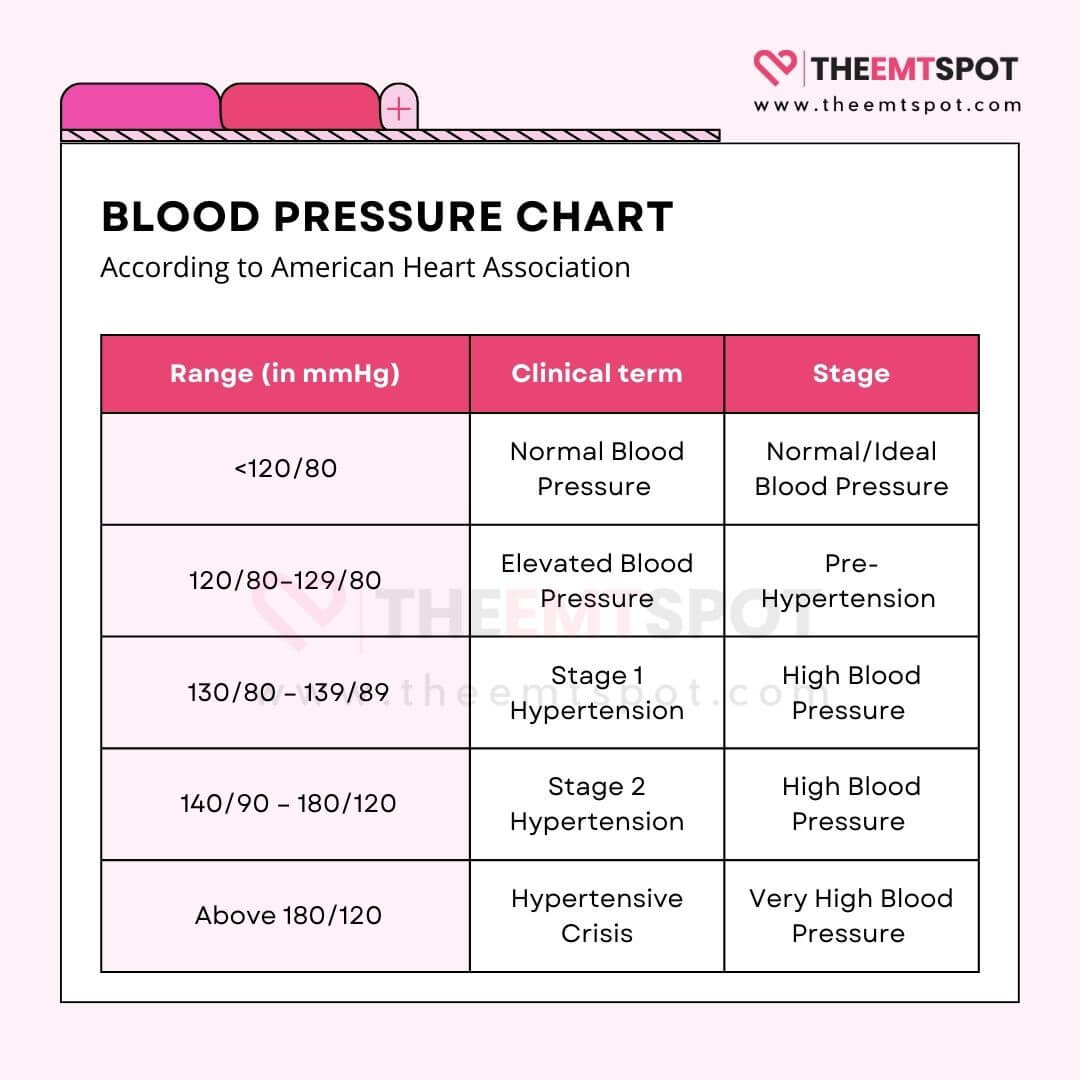
These charts can be customized for different demographics and are useful for tracking trends over time, which is essential for managing your health with the guidance of a healthcare provider.
How to take blood pressure at home?
If you wonder how to take blood pressure at home correctly, you may refer to the AHA guidelines.
According to it, to accurately measure your blood pressure at home, refrain from smoking, caffeine intake, and exercising 30 minutes before taking a reading.
Ensure you use a cuff that fits and place it on your bare arm, positioning yourself with a supported back and feet flat on the ground, arm at heart level, and cuff just above the elbow.
Relax for about five minutes prior to measurement without talking or using electronic devices. An empty bladder is also recommended for an accurate reading.
Consistently measure your blood pressure at similar times each day, and consult with your doctor if the average reading over a week is elevated.
Remember, occasional fluctuations are normal and not necessarily a cause for concern.
What are the best blood pressure machines?
The best blood pressure machines are those that are smart, portable, have good battery life, have superior cross-platform connectivity, and come with an app.
In this context, there are a few brands in the current marketplace: Oxiline, CheckMe, QardioArm, Omron, and Withings.
However, when hunting for the best, only two products outperform others in all segments due to their value for money and unparalleled features.

The first one is from the ever-popular Oxiline, manufactured by the US-based Oxiline LLC. Their Pressure X Pro is nothing short of a beast. Some of its highlight features are listed below.
- FDA 510(k) granted
- Mobile app support
- VIBRA™ TX Sensor for detecting arterial pressure
- Bluetooth connectivity
- Lifetime warranty
- Multi-user support
The second highlight product is a Shenzhen-based smart blood pressure monitor from CheckMe Care, well-known for its app interface and data infographics.

CheckMe BP2 has enough features to stand miles apart from others, as listed below.
- Mobile app support
- ECG with AI analysis
- Wi-Fi and Bluetooth connectivity
- Rechargeable
- OLED screen
- Real-time tracking
More in this topic






 Robin Backlund is a dedicated journalist and a medical student who has written several articles and essays exposing the falseness and hollowness of online resources in the medical science niche.
Robin Backlund is a dedicated journalist and a medical student who has written several articles and essays exposing the falseness and hollowness of online resources in the medical science niche.